
Nursing to Bottle Transition: Preemie Flow Control Compared

When navigating the nursing to bottle transition for premature infants, parents face a critical decision point: how to select bottles that honor the delicate feeding patterns developed in the NICU to home bottles journey. The infant feeding bottles available today vary significantly in flow control mechanisms, yet research shows that consistent flow rates matter more than packaging claims. In my years bridging ergonomics research and caregiver diaries, I've observed that babies give clear signals about what works, signals often overlooked when parents fixate on labels rather than latch angles. Watch the baby, not the box.
Why Flow Control Matters More for Preemies Than Term Infants
Premature infants develop oral-motor skills on a different timeline. Their coordination of sucking, swallowing, and breathing remains fragile during the transition from tube feeding to full oral intake. According to NICU feeding protocols, infants should demonstrate sustained suckling with swallowing for at least 5 minutes before transitioning to full breastfeeding or bottle feeding. During this vulnerable period, mismatched flow rates create unnecessary stress.
"In one toddler room I supported, two babies took identical bottles differently. One relaxed only when we widened the latch angle and slowed the flow; the other needed a narrower teat and faster pace."
Observable flow mismatch indicators:
- Coughing or choking within first 30 seconds of feed
- Falling asleep within 2 minutes (signaling flow too slow)
- Compressing nipple excessively (visible dimples at corners of mouth)
- Cheek dimpling during suck cycles
- Pushing bottle away after initial latch
These physical cues matter more than what's printed on the nipple packaging. "Preemie flow" on one brand might actually deliver faster flow than "Level 1" on another system due to inconsistent industry standards. Flow testing confirms this variability. What feels slow to one infant might overwhelm another.
How to Identify Flow Mismatch: Beyond the Marketing Labels
Premature infant bottle systems often fail when parents select based on age recommendations rather than observed feeding behavior. NICU bottle comparison studies reveal that actual flow rates can vary by as much as 40% between brands claiming identical flow levels. Instead of trusting "newborn" or "preemie" labels, observe these specific cues during feeding attempts:
- Pacing breaks: Does the baby consistently pause after 5-10 sucks? This suggests the flow exceeds their swallowing capacity.
- Lip seal: Blue-tinged lips during feeding indicate excessive negative pressure (baby working too hard to extract milk).
- Jaw movement: Noticeable jaw tremors or irregular movement patterns signal motor fatigue from flow mismatch.
- Post-feed alertness: A calm but awake baby after feeding suggests successful flow matching; excessive sleepiness may indicate flow too fast.

Dr. Brown's Preemie Flow Bottle Set
Dr. Brown's Preemie Flow system addresses this with their two-stage progression (Preemie Flow followed by Level T), allowing parents to match flow to observed infant readiness rather than arbitrary age guidelines. The internal vent system maintains consistent flow rates independent of bottle angle, a critical feature for preemies who lack head control.
Critical Bottle Features for NICU Graduates
When selecting preemie flow control solutions, focus on these evidence-based features rather than marketing claims:
Venting systems that prevent vacuum lock Preemies cannot generate enough negative pressure to overcome poor venting. Bottles with failed venting systems force infants to work harder, leading to fatigue and incomplete feeds. The Danish study referenced in CPS guidelines found that 62% of extremely preterm infants could suckle while on nCPAP when properly supported, a testament to their delicate respiratory needs. For a technical breakdown of how different vents maintain flow and reduce air intake, see our anti-colic bottle comparison.
Nipple geometry matching infant oral anatomy Look for nipples with:
- Shorter bases (12-15mm) to prevent over-insertion
- Gradual taper from base to tip (mimicking breast compression)
- Latch guides that encourage proper tongue positioning
Flow progression capability The ideal system allows gradual flow increases without changing bottle platforms. Dr. Brown's Preemie-to-Level T progression provides a 0.2mL/min increase between stages, clinically significant for preemies but subtle enough to avoid rejection.

PIGEON Baby Bottle Feeding Gift Set
Pigeon's approach incorporates latch-on line technology based on Japanese research into infant sucking behavior. Their SS nipple (0m+) features graduated firmness zones that respond to subtle pressure changes, a critical feature for preemies still developing oral strength. For full specs and performance with sensitive babies, read our Pigeon Peristaltic review.
Transitioning from NICU to Home Bottles: A Step-by-Step Approach
Hospitals vary widely in their use of bottle feeding for preemies. The Neo-BFHI guidelines recommend avoiding bottles until breastfeeding is established, using alternatives like cup feeding or supplemental nursing systems. However, for families needing to bridge to home bottle feeding, follow this evidence-based transition protocol:
Phase 1: Observe Feeding Readiness Cues
- Wait for coordinated suck-swallow-breathe pattern (typically 34-36 weeks corrected age)
- Notice rooting reflex strength, mature preemies will turn head purposefully toward stimulus
- Check for hand-to-mouth movements indicating oral exploration readiness
Phase 2: Single-Variable Testing Introduce one change at a time and observe:
- First, test bottle position (upright vs. side-lying)
- Second, test flow rate (keep position constant)
- Third, test pacing technique
Phase 3: Document Response Patterns Track in a simple diary:
- Time of day feeding attempts
- Position used (note angle relative to body)
- Flow rate indication
- Infant cues before/during/after
- Volume consumed

Paced Bottle Feeding: The Missing Link for Preemies
General tips for bottle-feeding emphasize holding babies side-lying with head slightly elevated, similar to breastfeeding position. For preemies, paced feeding becomes essential:
- Hold bottle horizontally so only the nipple fills with milk
- Allow 5-10 second pauses after every 10-15 sucks
- Follow infant's rhythm don't force continuous feeding
- Stop when the baby shows fullness cues (hand pushing, turning head)
Research shows paced feeding reduces oxygen desaturation events in preemies by 37% compared to traditional bottle feeding. For technique specifics on following your baby's cues, see our responsive bottle feeding guide. This technique prevents overwhelming their developing respiratory system while building oral motor skills.
Children's Colorado NICU recommends this approach specifically for preemies transitioning to oral feeds. The slower pace mimics natural breastfeeding patterns where milk ejection occurs in pulses rather than continuous flow.
What About Supplemental Nursing Systems?
The Medela Supplemental Nursing System (SNS) offers an alternative path for parents wanting to maintain breastfeeding while providing supplemental feeds. While not a direct bottle solution, it serves an important role in certain scenarios:
Best for:
- Infants with strong breastfeeding reflex but insufficient milk transfer
- Parents with low milk supply wanting to maintain supply through stimulation
- Non-gestational parents who wish to participate in feeding at breast
Limitations:
- Requires significant parental coordination skills
- Tube placement can interfere with proper latch
- Not suitable for infants with weak suck strength

Medela Supplemental Nursing System (SNS)
Actionable Next Steps for Your Preemie's Bottle Transition
Rather than cycling through multiple bottles hoping for acceptance, implement these evidence-based strategies:
-
Conduct a single-change experiment today: If using bottles with traditional nipples, try holding the bottle more horizontally during next feeding. Note if baby maintains latch longer or shows fewer fatigue cues.
-
Map your infant's current flow tolerance using this simple test: Fill a clean bottle with expressed milk, hold at 45-degree angle, and count how many drips occur in 10 seconds. <10 = slow flow; 10-20 = medium; >20 = fast. Compare to your current bottle's actual flow.
-
Request a feeding observation from your pediatric nurse or IBCLC. Professionals trained in infant feeding cues can identify subtle acceptance signals you might miss.
The truth is, no single bottle works for all preemies. If you want preemie-tested options vetted by specialists, start with these NICU bottles that fix preemie flow problems. What matters most is matching the system to your infant's observable comfort cues. As one NICU study demonstrated, infants transition to full breastfeeding faster when fed by syringe rather than bottle, proof that flow control mechanisms impact oral-motor development. But beyond the data stands a simpler truth: comfort cues predict acceptance better than labels or marketing tiers ever will.
Your next bottle choice shouldn't be based on what others recommend, but on what your baby tells you through their feeding behavior. When you watch the baby, not the box, you'll find the flow rate that turns feeding time from a battle to a bonding opportunity.
Related Articles


Adaptive Bottle Solutions for Parents With Disabilities

NICU Graduate Bottles for Medical Complexity: Flow Tested
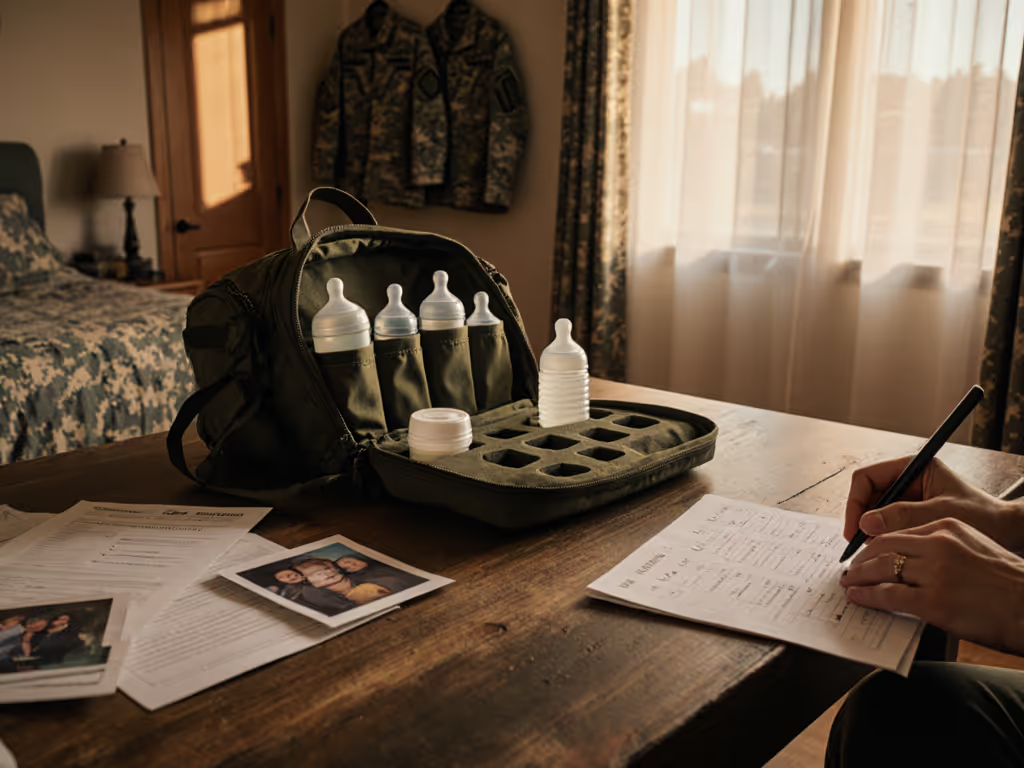
Military Family Bottle Solutions: Deployment-Ready Feeding

